Advanced Male Infertility Testing

At Maze Men’s Health, advanced treatment begins with a comprehensive semen analysis to identify the underlying causes of infertility and guide personalized care. Based on your results, we may recommend hormonal therapy, varicocele repair, or targeted lifestyle changes to improve sperm quality and reproductive health. For more complex cases, we offer microsurgical sperm retrieval, sperm banking, and coordination with IVF or ICSI specialists. Led by Michael A. Werner, MD, our team combines medical expertise with leading-edge technology to help men across Westchester, NYC, Connecticut, and New Jersey achieve their family-building goals.
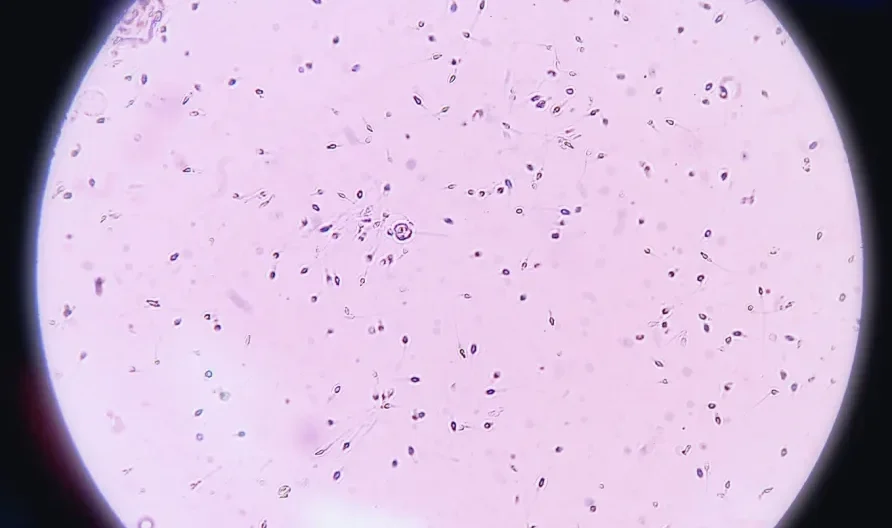
Semen Analysis
Semen is the fluid that a man ejaculates. It is produced at several different sites in the body. The sperm within the semen are the cells that actually fertilize the egg. While it is most important to assess the sperm, they account for only 1% to 2% of the semen volume. Problems with the surrounding fluid may also interfere with the movement and function of the sperm. Therefore, both the sperm and the fluid must be tested.
There is no specific, magic number of sperm in the semen analysis of men whose partners will get pregnant. The partners of some men with a very poor semen analysis may conceive easily. The partners of some men with an excellent semen analysis may experience difficulty. However, men with good semen analysis results will, as a group, conceive at significantly higher rates than those with poor semen analysis results. The semen analysis will help determine whether there is a male factor involved in the couple’s sub-fertility. In those cases, we will recommend an evaluation. There are certain findings of the semen analysis which suggest specific potential problems. For example, an increased white blood cell count may indicate infection or inflammation. However, other abnormalities in many of the main parameters are non-specific. For example, there are a number of different causes for a decreased sperm count or diminished sperm movement. Some of these causes have other serious medical implications, others don’t. A thorough evaluation helps determine the cause of an abnormal semen analysis.
Comprehensive Semen Analysis (Sperm Count, Motility & Morphology Testing)
Almost all laboratories will conduct tests and report on the following information, using values established by the World Health Organization:
Concentration (Sometimes Referred to as the Count)
Motility (Sometimes Referred to as Mobility)
Morphology
Volume
This is a measurement of the volume of the ejaculate. Normal is 2 milliliters (2 cc) or greater. The volume may be low if a man is anxious when producing a specimen, if the entire specimen is not caught in the collection container, or if there are hormonal abnormalities or ductal blockages.
Total Motile Count
Standard Semen Fluid Tests
Additional Semen Analysis Tests
Forward Progression
Kruger Morphology
Anti-Sperm Antibodies
White Blood Cells
The semen may contain a high number of white blood cells, which may be an indication of either infection or inflammation. White blood cells are considered significant if more than 1 million are found in each milliliter of the ejaculate.
White blood cells cannot be differentiated from other round cells normally found in the semen (debris and immature sperm) without special staining. If more than one-million round cells are found in the ejaculate, a portion of the ejaculate should be specially stained to look for an increased number of white blood cells.
If the white blood cell count is elevated, semen cultures should be performed on a subsequent specimen. Unfortunately, the semen culture cannot be performed on the original specimen as it must be the first step performed on the specimen in order to keep it sterile.
Specialized Semen Tests for Deeper Insights
In certain situations, specialized tests are needed. These depend on the findings at the time of the analysis and can often be performed on that specimen.
Spun Specimen
Viability
Sperm may be alive, but not moving. A specialized staining technique is used to determine what percentage of the sperm are alive and is indicated when the motility (percent moving) is less than 30%.
Fructose
Post-Ejaculatory Urinalysis (PEU)
ESSM (Extended Sperm Search & Microfreeze)
In 44% of cased where no sperm was found, this technique may be able to find even a single sperm through advanced processing techniques. These sperm may then be used in in vitro fertilization (IVF) with intracytoplasmic sperm insertion (ICSI). ESSM involves a specially trained andrologist processing the specimen, then dividing it into minute amounts. They then spends multiple hours looking through the entire semen specimen for any moving sperm. If sperm are found, they are placed on a specialized device, and frozen in a minuscule quantity of fluid so that they can be easily found when needed for insertion into an egg.