
I WAS JUST DIAGNOSED WITH AZOOSPERMIA. NOW WHAT SHOULD I DO?
A semen analysis showing azoospermia does not necessarily mean you won’t be able to have a biological child. Once the cause has been determined and the sperm production has been maximized, a number of procedures remain that can sometimes find sperm which can then be used with advanced reproductive techniques. It only takes one motile sperm per egg to potentially fertilize it.
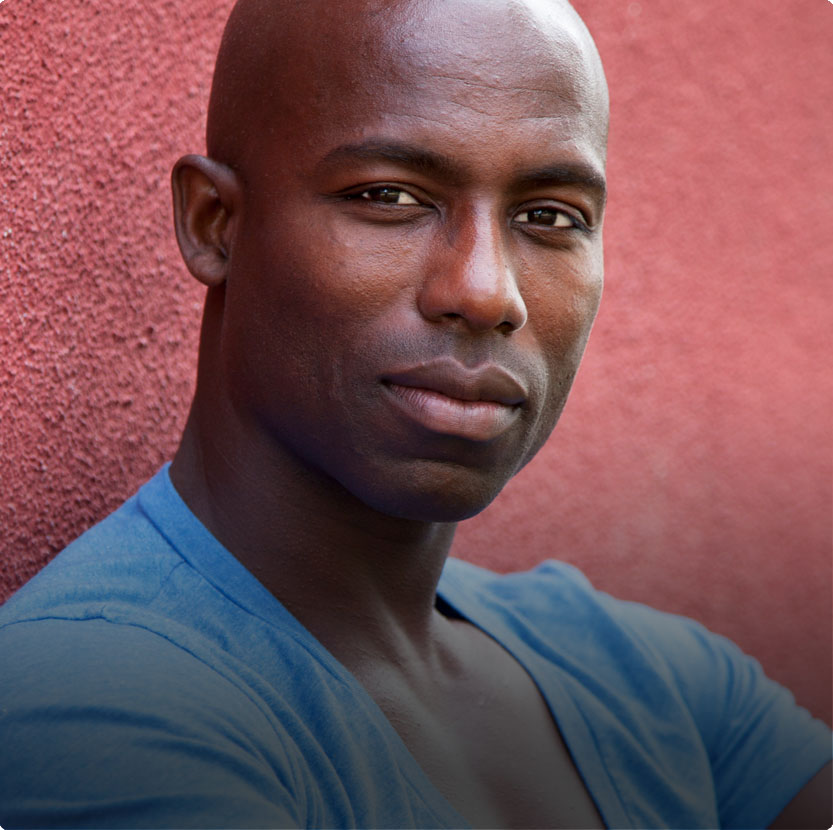
"We're reaching out to express our deepest thanks for your support in our fertility journey. The moment we stepped into your office was one of our biggest turning points. We were terrified, but your guidance, reassurance, and compassion during a time of extreme uncertainty for us meant more than words can express. Your ability to create an atmosphere of comfort and understanding sets a benchmark in patient care that is truly unparalleled." -- Patient Undergoing Fertility Treatment at Maze
If you've been diagnosed with Azoospermia or Cryptospermia and are interested in exploring your options, click through the chart below.
THE AZOOSPERMIA TREATMENT JOURNEY AT MAZE
The decision tree below explains how we approach a diagnosis of azoospermia. Click on any image or subject for more detailed information.

Azoospermia Diagnosis
Semen analysis with no sperm.
Azoospermia Diagnosis
At least two semen analyses should be performed in a sophisticated lab, before total azoospermia is diagnosed. We have often found sperm in men where other labs have found none. Also, since sperm production fluctuates in all men, some men with very low numbers of sperm may be periodically azoospermic.
Learn more about a Semen Analysis.

Evaluation By A Urology Specialist
A complete semen analysis and physical evaluation to determine the root cause of your infertility.
Evaluation By A Urology Specialist
The first step after receiving the diagnosis of azoospermia is an evaluation with a urologist specializing in male infertility to determine whether the cause is due to a problem with sperm production or sperm delivery.
Is it that the testes are not producing adequate numbers of sperm to see them in the ejaculate, or are adequate numbers of sperm being produced, but they can’t get into the ejaculate?
If sperm delivery is the problem, the next step is finding a way to retrieve sperm.
If sperm production is the problem, the next step is maximizing the sperm production.
Learn more about urologist Michael A. Werner, MD, founder and medical director at Maze Health.
Delivery Issue
Blockage (obstruction) or ejaculatory dysfunction.
Delivery Issue
If the testes are making adequate numbers of sperm but none are in the ejaculate (called “obstructive azoospermia” or OA), the sperm must be obtained by either restoring the normal flow of sperm through the full reproductive tract or retrieving it.
The following briefly describes causes and potential treatment options for delivery problems:
Absence of the Vas Deferens: Some men have a condition called Congenital (at birth) Bilateral (both sides) Absence of the Vas Deferens or CBAVD, which means they are missing both of the tubes that carry the sperm. Most of these men will carry two mutations for cystic fibrosis, a major and a minor one. Although this combination does not give them the disease, it does not allow the vas deferens to develop. Since this does not cause a problem with sperm production (unless there is another issue also occurring), sperm can be retrieved surgically from the testicle or the duct draining the sperm from the testicle, called the epididymis.
It is important that these men have genetic testing for cystic fibrosis mutations. If this mutation is found, his partner must be tested, and if she is positive for the mutation, then all embryos created should be checked prior to being transferred into the uterus to make sure they don’t carry both copies of the gene and would thus have the disease itself.
Obstruction of the Epididymis or Vas Deferens: Also, during examination of the ductal structures, the epididymis (which is the first part of the sperm carrying duct) may feel as though it is enlarged and/or firm. Generally, it is flat, and the middle cannot be felt. If the epididymis is enlarged and hard, there may be a blockage.
Likewise, the vas deferens may have become blocked from infection or surgery (including a vasectomy.) This can sometimes be felt during the exam.
Treatment Options for Blockage/Absence of the Vas Deferens or Epididymis
As described above, a man may be missing the tubes that carry the sperm, Congenital Absence of the Vas Deferens. He may have obstructions either at the level of the delicate tubular structure draining the testes (the epididymis) or higher up in the more muscular vas deferens. He may have become mechanically blocked during hernia or hydrocele repairs. Of course, a previous vasectomy would be known cause of ductal obstruction.)
Vasal Reconstruction: In certain cases, the flow of sperm through the reproductive tract can be re-established. The most common case is after a man has a vasectomy (though sometimes it can be done after a man has a blockage from an epididymal infection.) If this is successful, it may be possible for his partner to conceive naturally through intercourse, and not need IVF/ICSI. Success rates vary by length of time since the vasectomy, and the findings during the surgery.
Sperm Retrieval: If there is evidence that the sperm are being made (based on testicular size, the rest of the scrotal exam, and hormonal profile) but can’t get out, a specialist can go in and get (retrieve) the sperm. However, the numbers retrieved are low and the sperm themselves move slowly, so this must be combined with in vitro fertilization, and injection of an individual sperm into each egg. The two main options for sperm retrieval are:
Micro Epididymal Sperm Aspiration (MESA): This procedure is done by the specialist in the operating room, under light anesthesia. An incision is made in the scrotum, and the epididymis isolated. Using an operating microscopic, the urologist makes a small incision in the tubule of the epididymis and then has his lab specialist look at the fluid under a regular microscope to see if there are moving sperm. This may be done in multiple locations of the scrotum and possibly on both sides until adequate sperm are retrieved.
The sperm are frozen in multiple vials, which means that it is very rare that a second procedure would be needed for subsequent IVF/ICSI procedures if performed.
Also, it can be done in advance of the partner’s egg retrieval, which makes scheduling much easier. Frozen sperm, if moving when thawed, produces the same results as freshly retrieved sperm.
Needle (Percutaneous) Testicular Biopsy: The day before his partner’s eggs are to be retrieved, the man comes to his urologist’s office for this very simple procedure. The nerves leading to the testis are injected with a local anesthetic, as is the skin. A small skin incision is then made.
A biopsy core is taken of the testis, placed in specialized fluid, and then a drop is examined for sperm. The testis is then compressed for five minutes to stop bleeding. The next day, individual sperm are taken by the embryologist at the wife’s doctor’s lab and injected in her eggs. The advantage of this procedure is that it is less invasive than a MESA, does not require an anesthesiologist or hospital, and is cheaper. The disadvantage is that often there are only enough sperm for the one IVF cycle, and it may need to be repeated in the future.
Treatment Options for Ejaculatory Duct Obstruction
Sperm are stored in sacs called the seminal vesicles, and then are deposited in the urethra, which is the tube through which men urinate and ejaculate. The sperm must pass through the ejaculatory ducts to get from the seminal vesicles to the urethra. If these are blocked on both sides, no sperm will come through, even if some fluid does.
Trans-Urethral Resection of the Ejaculatory Duct (TURED): A cyst, in some cases, may be unroofed by operating through the urethra to open it, thus decompressing the ejaculatory duct. If the blockage occurs within the ejaculatory duct, the blocked part may be removed in a similar operation. In some cases, this results in normal amounts of sperm being ejaculated, and a pregnancy can occur through natural intercourse, or intrauterine inseminations.
Treatment Options for Ejaculatory Dysfunction
There may be problems with ejaculation. Before a man ejaculates, the sperm must first be deposited in the urethra. This process is called emission. There may be neurological damage from surgery, diabetes, or spinal cord injury that prevents this from happening. Also, for the sperm to be pushed out the tip of the penis, the entry to the bladder must be closed, which happens naturally and unconsciously during normal ejaculation. If it does not close, the sperm will be pushed into the bladder (rather than out the tip of the penis) and then subsequently washed out when the patient urinates.
Medications for Ejaculatory Dysfunction: There are many suggested medications and regimens to get men to deposit the sperm in their urethras with orgasm (emission) and to convert them from ejaculating backwards into the bladder, to forward, out the tip of the penis.
We most commonly use pseudophedrine 30mg immediate release tablets. (These are the ones that are kept behind the pharmacy counter, but don’t need a prescription. They are tracked as they are a needed component for crystal meth.) Regimens vary. Other medications used include imipramine, midodrine, ephedrine, phenylephrine, and chlorpheniramine.
After an orgasm, the man should milk his urethra into a specimen cup to see if any fluid comes out. This sometimes has enough sperm to be frozen (cryopreserved) and avoid the necessity for sperm retrieval procedures. Unfortunately, this is often unsuccessful, and sperm retrieval is necessary.
Unfortunately, this is often unsuccessful, and sperm retrieval is necessary.
Post Ejaculatory Urinalysis (PEU): It is possible that ejaculation is occurring “backwards”; instead of the ejaculate being pushed forward and ejaculated out of the tip of the penis, the sperm is being pushed into the bladder. This is not medically dangerous. The ejaculate is washed out the next time the man urinates.
To test for this, we have the patient empty his bladder and then ejaculate into a cup. He is then asked to urinate again into a different specimen container, which tested for sperm. This is called the post ejaculatory urinalysis. If there are significantly more sperm in his urine than his ejaculated specimen he has ejaculated backwards. Sometimes, this can be corrected by oral medication. If not, the urine can be prepared so that it does not damage the sperm as much, and the sperm is then harvested from the post-ejaculatory urine.
Transrectal Ultrasound: In order to rule out a blockage of the ejaculatory duct, an ultrasound of the ejaculatory duct and seminal vesicles is often performed. In this test, the ultrasound probe is placed in the rectum since the ducts lie near the rectal wall. Also, the ejaculatory duct traverses the prostate (a gland that can be felt through a man’s rectal wall.) If the seminal vesicles are dilated, this indicates that they may be full of semen because they cannot empty properly. Cysts blocking the ejaculatory ducts by exerting pressure on their walls, or calcifications in the ejaculatory ducts themselves, may also be noted. A cyst, in some cases, may be unroofed by operating through the urethra to open it. This decompressing the ejaculatory duct. If the blockage occurs within the ejaculatory duct, the blockage may be removed in a similar operation.

Production Issue
Testes are producing very few or no sperm.
Production Issue
If the testes are not producing adequate sperm to see them on a regular semen analysis (called “non-obstructive azoospermia” or NOA), we need to explore whether treatment can make the sperm production better, even to the point of finding just a few sperm on the Extended Sperm Search & Microfreeze (ESSM) procedure. If no sperm are found with ESSM, a relatively non-invasive technique called Sperm Mapping can help predict whether sperm would be found using a more invasive technique where the sperm are actually harvested from the testes called a micro-TESE.
Some causes of sperm production problems may be reversible, such as hormone imbalance or a varicocele. If the urology specialist does not find any reversible causes for the patient’s azoospermia, attempts to maximize production will not be useful. In some rare cases, genetic testing (i.e. certain Y microdeletions) may show that it is impossible for the man to produce sperm and therefore, all further attempts at treatment and sperm retrieval should be abandoned.
The following briefly describes causes and potential treatment options for production problems:
Physical Examination: The first step in the evaluation is the physical exam. Since most of the bulk of the testes is comprised of sperm producing elements (the seminiferous epithelium), if the size of the testicle is severely diminished, this is usually because of issues with the sperm producing part of the testicle. Many men with small testes and problems with sperm production still have normal testosterone levels, though many will not. This is because the testosterone is made by a different type of cells in the testes, called Leydig cells.
Hormonal Evaluation: Follicle stimulating hormone (FSH) is the hormone, made by the pituitary, which is responsible for stimulating the testes to make sperm. When the sperm-producing capacity of the testes is diminished, the pituitary makes more FSH in an attempt to make the testes do their job. Therefore, if a man’s FSH is significantly elevated, there is a strong indication that his testicles are not optimally producing sperm. If a man has a very low FSH, then he is lacking the ability to make FSH, which is needed by the testis to promote sperm production. This may actually be good news in terms of treating the azoospermia, as many men have sperm in the ejaculate after treatment with FSH.
Testosterone, estradiol, prolactin, luteinizing hormone (LH), and thyroid stimulating hormone (TSH) are also measured to assess a man’s hormonal status. These may reveal problems that can significantly impact sperm production. It is crucial that a man not go on testosterone replacement therapy, as this will shut down the production of sperm in the testes. The only way to get the high concentration of testosterone in the testes needed to make sperm, is for the testosterone to be made in the testes itself.
Men who take androgens (steroids) for body building, either by mouth or injection, shut down the production of hormones needed for sperm production, and thus often shut down sperm production completely or decrease it significantly. Fortunately, this can almost always be reversed.
A prolactin-producing tumor, a prolactinoma (which fortunately is almost never metastatic and usually treated with medication), can significantly decrease sperm production.
Thyroid problems can also have a negative effect on sperm production.
Treatment Options: The most common hormonal treatment for men with a testosterone level of less than 400 is selective estrogen receptor modulator (SERM) or Clomiphene Citrate. This pushes the pituitary gland to make more FSH and LH, which in turn pushes the testes to (try to) make more sperm and testosterone. The man may also notice that he feels better, since a higher testosterone level may help energy level, libido, muscle mass, erections etc.
Genetic Testing: It is recommended that all azoospermic men receive basic genetic testing, called a karyotype, which measures the number of chromosomes and looks at the large blocks of genetic material to make sure they are correctly aligned in the proper chromosome. Extra chromosomal material, or chromosomal material improperly aligned, can have a significant effect on sperm production.
There are tests for specific genetic abnormalities on the male (Y) chromosome in the areas that code for sperm production that can cause low levels of sperm or complete and irreversible azoospermia. These mutations are called Y microdeletions. If a son were to inherit one of the mutations that caused a significant decrease in sperm production, he would be expected to have the same problem.
Screening for the mutations that can cause cystic fibrosis is sometimes suggested. If present, it can cause problems with the sperm ducts.
Varicoceles: The scrotum is examined for the presence of dilated veins, called varicoceles, which can suppress sperm and also testosterone production. Their presence can be confirmed by a scrotal ultrasound, which is done non-invasively by applying a probe to the scrotal skin.
There are several ways to fix a varicocele. However, studies show that the microscopic sub-inguinal varicocelectomy with ultrasound guidance is the most effective procedure. This can only be performed by a urologist specializing in fertility and microsurgery, such as Doctor Michael Werner at Maze.
44% of men with azoospermia are found to have sperm after a varicocelectomy is performed and more than one in eight will go on to achieve a pregnancy naturally. As a result, a man with a varicocele and azoospermia should not be considered azoospermic until after a varicocelectomy is performed.
Testicular Failure Causing Azoospermia: In general, this means that the sperm-producing part of the testicle (the seminiferous epithelium) isn’t making adequate numbers of mature sperm. This failure may occur at any stage in sperm production for several reasons. Either the testicle may completely lack the cells that divide to become sperm (this is termed “sertoli cell-only syndrome”) or there may be an inability of the sperm to complete their development (this is termed a “maturation arrest.”) This situation may be caused by diagnosable genetic abnormalities. The screening for this must happen prior to any other diagnostic or therapeutic procedures. However, often we cannot find a reason for testicular failure.

Sperm Retrieval
Performed for obstruction and coordinated with partner’s egg retrieval for IVF.
Sperm Retrieval
If there is evidence that sperm are being produced but can’t get out, a urologist specializing in male infertility can retrieve the sperm. Often, this can be done with a simple needle biopsy, in the office, with a local anesthetic. Extra sperm can be frozen with a high chance of both being able to find them and of surviving the freeze and thaw process, if the tissue is processed using Extended Sperm Search & Microfreeze (ESSM).
Another option is to go into the epididymis surgically; though this is a more invasive procedure, it often yields more sperm, which can be successfully frozen using conventional freezing methods. However, in all cases of surgically retrieved sperm, these sperm can only be used with in-vitro fertilization (IVF), and injection of an individual sperm into each egg.

Maximize Sperm Production
Hormone treatment and varicocelectomy.
Maximize Sperm Production
In men with production issues (Non-Obstructive Azoospermia or NOA), the first step is to try to increase sperm production, usually hormonally or through varicocelectomy. In certain cases, the urology specialist may diagnose a varicocele, which is a group of dilated veins in the scrotum. Fixing these, through a varicocelectomy, may improve sperm production, sometimes to the point where sperm are seen in the ejaculate.
Hormones must also be checked. Sometimes hormonal treatment is indicated, and can lead to sperm in the ejaculate.
If the sperm production has been increased but a conventional semen analysis is still not finding sperm, an Extended Sperm Search & Microfreeze (ESSM) is performed. Sperm can be found, isolated, and frozen 44% of the time using ESSM.
If the ESSM is unsuccessful, a Sperm Mapping is recommended. This is a relatively non-invasive diagnostic procedure to determine if sperm are likely to be found for use on the more invasive open micro-TESE.

Perform An ESSM
In 44% of azoospermic patients, sperm have been found and successfully frozen.
Perform An ESSM
Extended Sperm Search & Microfreeze (ESSM) may be able to find sperm that even a careful conventional semen analysis with a post ejaculatory urinalysis can’t find. This may be because the numbers are so low, that they are not seen in a random drop of sperm used for a conventional semen analysis. Even if the specimen is spun down with a centrifuge, and the pellet at the bottom evaluated, unless every drop is looked at thoroughly, individual sperm may be missed.
As the only lab in the US offering Extended Sperm Search and Microfreeze (ESSM), Maze has found and frozen motile sperm in 44% of azoospermic men. These sperm may then be used in in-vitro fertilization (IVF) with intracytoplasmic sperm insertion (ICSI). ESSM involves a specially trained andrologist processing the specimen, then dividing it into minute amounts. They then spend multiple hours looking through the entire semen specimen for any moving sperm. If sperm are found, they are picked up using a micromanipulator and individually placed on a specialized freezing dish in a small amount of fluid. This device allows for a freezing and thawing technique with excellent preservation of sperm motility and makes it very easy for the embryologists to find and place into an egg. Learn More

Find & Freeze Sperm
Inject sperm found on ESSM into a freshly retrieved or frozen egg.
Find & Freeze Sperm
If sperm are found and frozen using ESSM, they are then able to be thawed and injected into oocytes by your IVF center. We can send the frozen specimens anywhere in the country, as well as internationally, and teach embryologists how to thaw and use the sperm. For clinics that are local to our area, we can do an ESSM the day of egg retrieval, and send fresh moving sperm in small wells to be injected directly into the eggs.

No Sperm Found
Negative ESSM. Some men may still have sperm retrieved directly from the testes.
No Sperm Found
In those cases where appropriate interventions have been tried and where the ESSM did not locate sperm in the ejaculate, there may be the possibility of harvesting sperm directly from the testes.
In 43-68% of azoospermic men there may be a small number of sperm, which have been produced in the testis, but exist in such small quantities that they do not reach the semen.
The traditional way to retrieve sperm is through an invasive procedure in the operating room, called a microscopic testicular sperm extraction (micro-TESE). However, for many years we have preferred sperm mapping, as a diagnostic tool to see if there are actually sperm in the testicle, before proceeding with micro-TESE and having a partner go through an IVF cycle.

IVF/ICSI
Injecting individual sperm directly into an egg.
IVF/ICSI
The only way to use individual sperm is by injecting them directly into an egg (ICSI). This egg can be freshly retrieved during an IVF/ICSI cycle, or frozen. It can be from the female partner or from a donor.
If an ESSM has been performed, the sperm can be retrieved from a frozen Sperm VD. For IVF centers that are local, fresh specimens can be retrieved on the day of egg retrieval.
Sperm Mapping + ESSM = GN-SEM
Aspirating sperm directly from the testes with fine needles.
Sperm Mapping + ESSM = GN-SEM
We have recently pioneered the use of combining the diagnostic value of the sperm mapping with the therapeutic value of collecting sperm at the same time using ESSM. We have termed this Grid Needle Sperm Extraction and Microfreeze or GN-SEM.
For traditional sperm mapping, a “map” is drawn on the scrotal skin, and sequential needle aspirates/biopsies taken from designated demarcated sites. Each one is placed on a marked slide, and then they are all sent to a pathology lab, to see if there are any sperm present, and if so, where they are located. The sperm would then traditionally be procured using an invasive procedure called a micro-TESE. This process requires aspirating sperm from the testes twice.
With this new procedure, we have pioneered the use of simply placing a biopsy needle into the area where sperm are predicted but instead of putting them on a slide, we are putting them in fluid hospitable to sperm. We then do an ESSM on the fluid containing the aspirates, and if sperm are found they are then frozen for later use.
Thus, in one dramatically less invasive procedure, we are not only diagnosing whether there are sperm in the testicles but procuring them for use with IVF/ICSI simultaneously. Learn more about this revolutionary new protocol!

No Sperm Found
Negative results with various sperm retrieval methods.
No Sperm Found
If no sperm are found after a definitive sperm retrieval technique is performed, the man or couple must decide how to proceed.

Find Sperm, IVF/ICSI
Live sperm can be individually injected into a fresh or frozen egg.
Find Sperm, IVF/ICSI
The only way to use individual sperm is by injecting them directly into an egg (ICSI). This egg can be freshly retrieved during an IVF/ICSI cycle, or frozen and can be from the female partner or from a donor.
If an ESSM has been performed, the sperm can be retrieved from a frozen Sperm VD or fresh specimens on the day of egg retrieval, for IVF centers that are local.

Options
Designated donor sperm, anonymous donor sperm, adoption, or a child-free life.
Options
As a reproductive urologist who also runs a reproductive urology laboratory, my patients’ primary goal is for me to help them have a biological child. However, if definitive sperm retrievals have been performed without sperm found, different options must be considered. Many couples are initially adamant that they will not using any sperm but the man’s own. In my experience, this often changes when faced with the reality that he produces no sperm. Some of my happiest families are those created with donor sperm. Support groups exist to help you navigate this decision.
Designated Sperm Donor:
Maze Labs is one of the few labs who are licensed to store the sperm of “designated donors.” This means that a man is chosen, by the parties who want to start a pregnancy, to donate his sperm for this purpose. It can be a heterosexual couple, gay couple, or a single man or woman. New York State and federal law require that testing for STI’s and genetics be performed and a physical exam be done. It is a complicated process on the lab’s part, but relatively easy for the donor.
Anonymous Sperm Donor:
A couple may obtain sperm from a donor unknown to them previously, from a sperm bank. A comprehensive list of these banks can be found here: SpermBankDirectory.com. These donors are carefully screened. Now with public genetic testing the anonymity of the donors is of course changing.
Adoption:
Unfortunately, this option has become more and more expensive, time consuming and difficult, especially for newborns.
Child Free Living:
Many couples decide on this option, and many for religious reasons.
WHY SHOULD I CHOOSE MAZE HEALTH?
Men facing a semen analysis often fear the diagnosis of azoospermia. However, that diagnosis does not necessarily mean that the man will never have a biological child. Accurate diagnosis, evaluation, treatment, and management of azoospermia is complicated and should be performed by a specialist in male infertility.
A complete diagnostic evaluation must be performed to determine whether the issue is a production (non-obstructive azoospermia) or delivery (obstructive azoospermia) problem. If the issue is in the delivery of the sperm, the focus is on retrieving, and often freezing the sperm. If the issue is a production problem, the first step is to attempt to maximize sperm production (usually through hormonal treatment or varicocelectomy, if appropriate.)
At Maze, our expert team led by board-certified Urologist Michael Werner, MD, performs a thorough evaluation, including blood testing and analysis, followed by development of a customized treatment plan that we will create together. This decision tree above provides examples of options we may include in your plan, as well as others based on your specific needs.
IN A PATIENT'S OWN WORDS:
We have been trying to conceive for over ten years now and honestly we were close to the end of the road before we came to Maze. I have done sperm analysis’s over fifteen times in four different countries. All with the same disappointing result; azoospermia. After every test I took I would wish for at least one sperm to be found just as a sign of hope but I was always told there is nothing. I have been to the top urologist in this country and their only solution would be a surgery. My wife and I were against the surgery unless we have exhausted all other options.
I say faith brought us to you. I did the test in the morning in Manhattan and was expecting a call the next day or two as usual with the usual disappointing news of azoospermia. I remember getting a call later that evening from a New York number and did not even think it was you. I answered that call that changed our life for the better. I remember you telling me that, “I have good news for you we were able to freeze over 40 sperm.” and I could not believe my ears. I remember asking you if you’re sure you called the right person!!! It was the greatest news I had ever received in my life to say the least. I did a few more tests with positive results to ensure we have enough just as a safety net even though you told me it’s enough to conceive.
I’m glad to announce that this year we had a beautiful baby boy after a few failed IVF procedures who is the center of our lives now. I ultimately hope that you are able reach as many people as possible with your innovative techniques and dedication to your skills. Your emotional support was beyond what we expected and much appreciated. This is only a fraction of our gratitude for you and your facility for everything you have done for my family.
Thank you from the bottom of our hearts…
– FK, 37 –
Read more testimonials here.
Last Updated: June 2023
